Lipoprotein(a) (Lp(a)) is a plasma lipoprotein consisting of an LDL-like particle in which apolipoprotein B100 (apoB100) is covalently linked to the plasminogen-like protein, apolipoprotein(a) (apo(a)).1,2 As apo(a) occurs in many different sizes, with more than 40 different isoforms, Lp(a) particles also occur in more than 40 different sizes – uniquely amongst circulating proteins.3 Over 80% of people carry two different sized apo(a) isoforms, each inherited from one parent; typically, the smallest form predominates in plasma.3
Lp(a) is produced mainly in the liver, and is thought to play a role in wound healing though, as some people have undetectable levels, its physiological significance is uncertain.1
Lp(a) is less than 70 nm in diameter and can pass freely across the endothelial barrier and remain within the arterial wall,4 as a result of strong interactions with extracellular matrix components within the arterial wall. It has a range of pathological properties, including atherogenic, thrombogenic and pro-inflammatory effects.1,5
Lipoprotein(a) particle structure
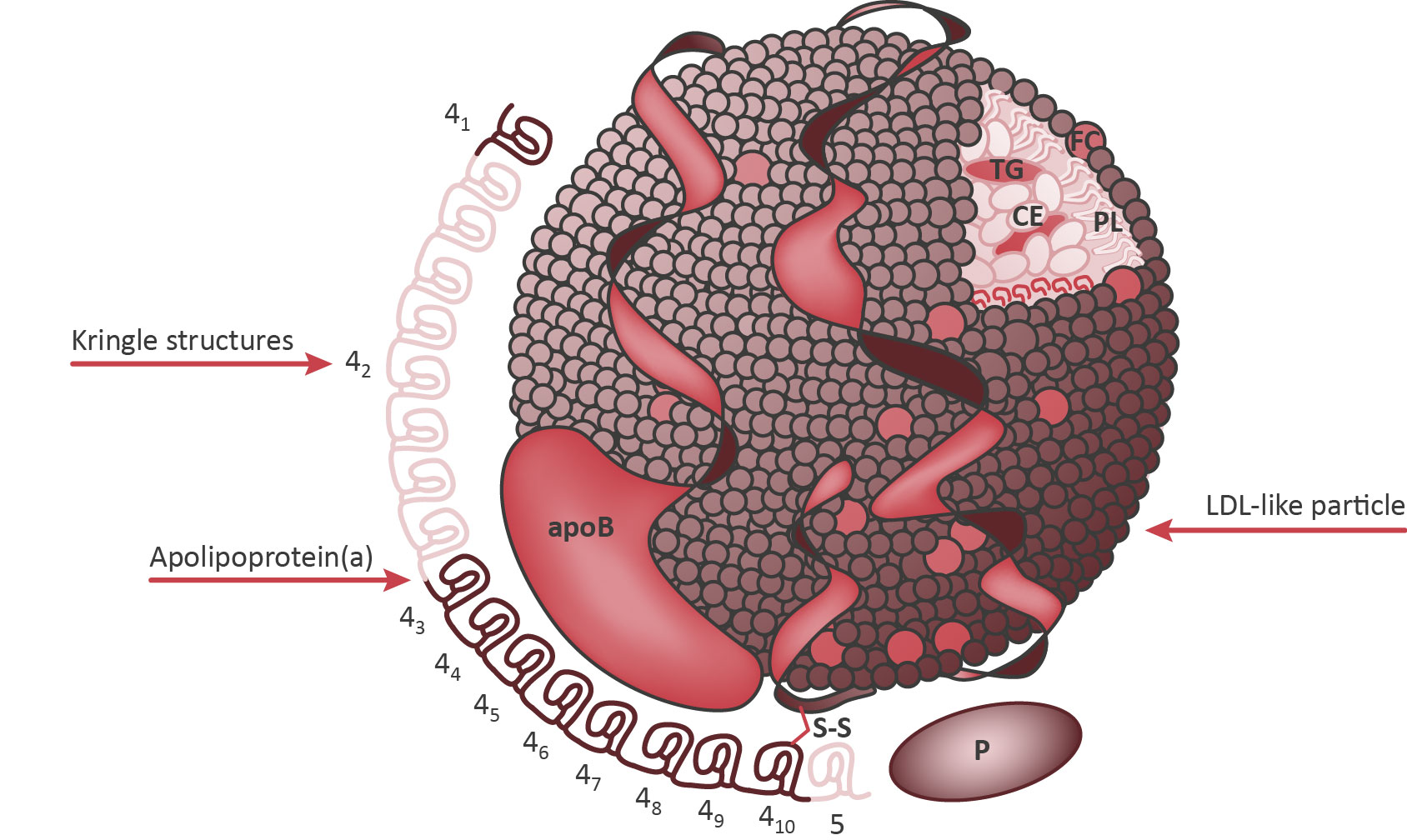
Reproduced with permission: Koschinsky M, Marcovina S. Structure-function relationships in apolipoprotein(a): insights into lipoprotein(a) assembly and pathogenicity. Curr Opin Lipidol 2004;15:168.
| Pro-atherogenic properties | Prothrombotic properties |
|---|---|
| ↑ Oxidized phospholipids ↑ Foam cell formation ↑ Endothelial dysfunction ↑ Smooth muscle cell proliferation ↑ Chemoattraction of monocytes ↑ Inflammation of the arterial wall | ↓ Plasminogen activation ↓ Fibrinolysis ↓ Tissue factor pathway inhibitor ↓ Clot permeability ↑ Platelet response |
Lp(a) concentration is determined mainly by genetic factors, with the LPA gene fully expressed by the age of two years.6 Adult levels are generally reached by the age of five years, though they may increase into adulthood.6 The Kringle-IV (K-IV) repeat polymorphism is responsible for approximately 30-70% of the variability in Lp(a) concentration. Expression of fewer than 23 K-IV repeats is characterised by small apoA isoforms, and these are associated with raised Lp(a) concentration compared with large apoA isoforms.6
Mendelian randomisation approach demonstrating a causal association between
Lp(a) levels and CVD
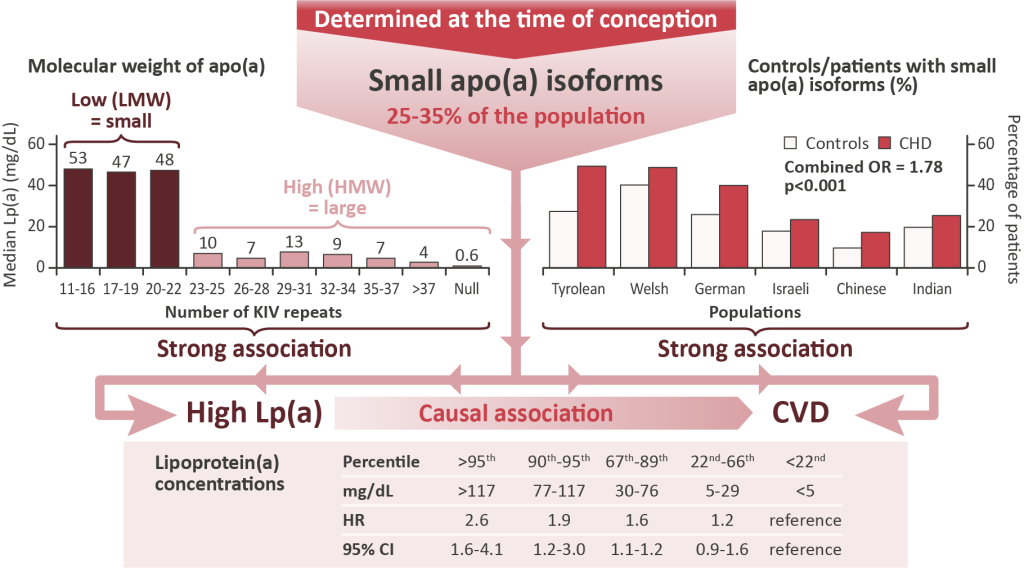
Adapted from Kronenberg, Handbook Exp Pharmacol, 2021; Kamstrup et al, 2009
Composition of Lp(a)
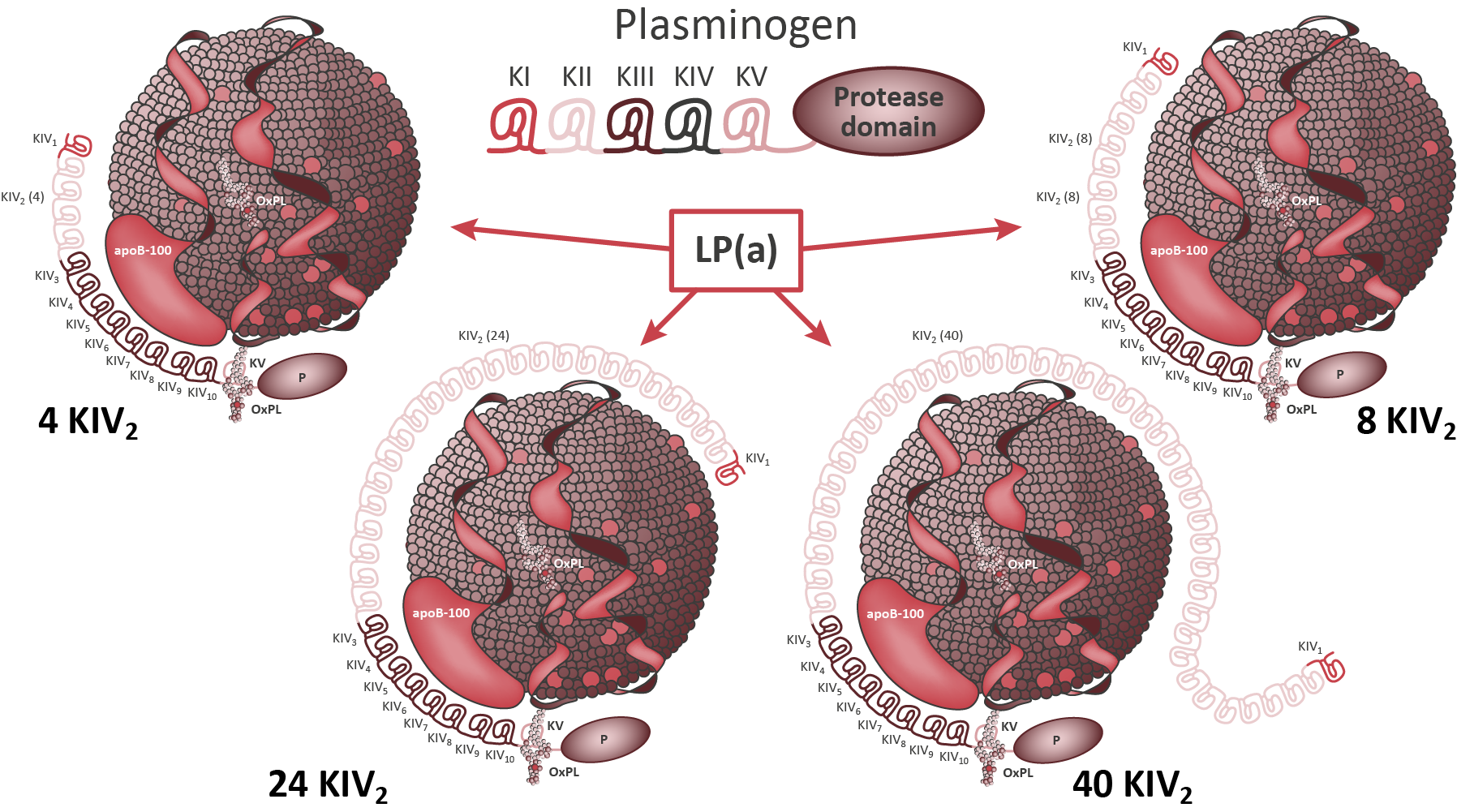
Adapted from Tsimikas, S. (2017). A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. Journal of the American College of Cardiology, 69(6), 692-711. https://doi.org/10.1016/j.jacc.2016.11.042
However, this inverse relationship between isoform size and Lp(a) concentration may be modified by a variety of LPA variants.5 APOE, CETP, and APOH loci are also associated with Lp(a) concentration.5
Non-genetic factors may also affect Lp(a) levels:6,7
- Factors that may increase Lp(a) levels: high carbohydrate diet, hypothyroidism, pregnancy, chronic kidney disease, severe inflammatory conditions, fine particle air pollution
- Factors that may decrease Lp(a) levels: low carbohydrate diet, hyperthyroidism, postmenopausal hormone replacement therapy, hepatic impairment (depending on cause), sepsis, severe burns, tocilizumab (interleukin 6 inhibitor)
Sex and ethnicity also affect Lp(a) levels, with typical concentrations approximately 5-10% higher in women than men, and higher in black and South Asian populations than white and Chinese populations.4 In women, Lp(a) levels tend to increase at the menopause.4
References
- Alebna PL, Mehta A. An Update on Lipoprotein(a): The Latest on Testing, Treatment, and Guideline Recommendations. American College of Cardiology, 19 September 2023
- Koutsogianni AD, Liamis G, Liberopoulos E et al. Effects of Lipid-Modifying and Other Drugs on Lipoprotein(a) Levels-Potent Clinical Implications. Pharmaceuticals (Basel). 2023 May 16;16(5):750
- Tsimikas S. A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies. J Am Coll Cardiol. 2017 Feb 14;69(6):692-711.
- Mach F, Baigent C, Catapano AL et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188.
- Kronenberg F. Lipoprotein(a). In: von Eckardstein, A., Binder, C.J. (eds) Prevention and Treatment of Atherosclerosis. Handbook of Experimental Pharmacology 2021; 270. Springer, Cham. https://doi.org/10.1007/164_2021_504
- Kronenberg F, Mora S, Stroes ESG et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J. 2022 Oct 14;43(39):3925-3946.
- Enkhmaa B, Berglund L. Non-genetic influences on lipoprotein(a) concentrations. Atherosclerosis. 2022 May;349:53-62.




